If HDL is the “good” cholesterol, shouldn’t more always be better? Not exactly. HDL’s job is to carry excess cholesterol away from your arteries back to the liver—a clean-up service called reverse cholesterol transport. A healthy HDL level helps lower heart attack and stroke risk, but HDL doesn’t erase high LDL (“bad”) by itself—the rest of your lipid picture still matters.
What “low HDL” really signals inside your body
When HDL runs low, your “clean-up crew” is smaller and the balance tilts toward artery plaque build-up over time. Low HDL often travels with high triglycerides, insulin resistance, central weight gain, and higher blood pressure—the cluster doctors call metabolic syndrome. That combination, not the HDL number alone, is what drives risk upward.
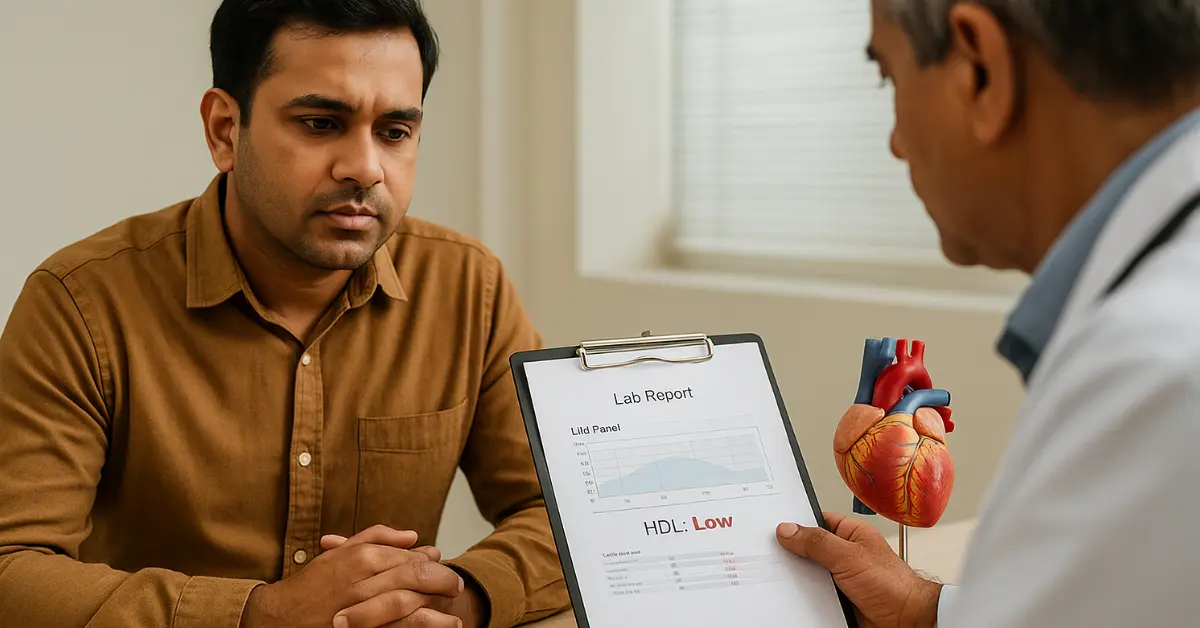
Key point: Low HDL usually has no symptoms—it shows up on a lipid panel. The danger is the long-game: more plaque, stiffer arteries, higher odds of heart attack or stroke unless you change the overall risk pattern.
How low is “low”?
Typical cut-offs used in clinics:
- Men: HDL < 40 mg/dL is low
- Women: HDL < 50 mg/dL is low
Many labs also flag ≥ 60 mg/dL as “protective.” Your clinician interprets this alongside LDL, non-HDL, triglycerides, blood pressure, diabetes status, smoking, and family history.
Why HDL goes low (the usual culprits)
- Inactivity and excess weight (especially belly fat)
- Smoking/vaping
- High refined carbs/added sugars → high triglycerides
- Type 2 diabetes/insulin resistance
- Genetics (some people are wired for lower HDL)
These factors are routinely linked with lower HDL on AHA/CDC guidance—and the good news is that most are fixable.
The part nobody tells you: “Raise HDL” isn’t the main goal
Big trials and modern guidelines don’t recommend chasing HDL with pills. For example, niacin raises HDL on paper but hasn’t consistently reduced events, and side effects are common. Today’s playbook is to drive LDL/non-HDL down and tame triglycerides—that’s what reliably cuts risk. HDL generally improves function inside that healthier pattern.
Related Article : How to raise HDL Cholesterol naturally?
What to do next: a 7-step fix that actually moves risk
- Move most days (duration wins).
Aim for 150–300 minutes/week moderate aerobic activity (e.g., brisk walking, cycling, swimming) plus 2 strength days. This combination modestly lifts HDL over time and improves triglycerides, blood pressure, and insulin sensitivity. - Swap fats—don’t stack them.
Replace butter/ghee and creamy sauces with olive, groundnut/peanut, mustard, or canola oil—and measure total oil to ~1–2 Tbsp/day depending on calories. Diets lower in saturated fat and free of trans fat improve your overall lipid profile. - Add soluble fiber daily.
Target 5–10 g/day from oats, barley, pulses (chana/rajma/masoor), apples/pears. Soluble fiber pulls LDL down and supports a better risk profile even if HDL rises only a little. - Bring in omega-3s.
Eat fatty fish (sardines/mackerel/salmon) 2–3×/week, or add flax/chia/walnuts most days. Omega-3s help triglycerides and support HDL’s protective role within a heart-healthy pattern. - Trim sugars/refined carbs.
Swap sweet drinks, sweets, and ultra-refined snacks for fruit, curd with seeds, or a handful of nuts. High triglycerides and low HDL often show up together—cutting sugar helps both. - Quit smoking/vaping.
Stopping tobacco use raises HDL and improves HDL function—another reason to make this the month you quit. - Treat LDL/non-HDL first.
Many adults aim for non-HDL < 130 mg/dL (lower targets if you have heart disease or diabetes). Talk to your clinician about lifestyle plus medication when indicated—because lowering LDL/non-HDL is what cuts events.
What “happens” over time if you don’t change course
- Plaque builds faster as LDL hangs around; arteries grow narrower and less flexible.
- Triglycerides creep up, HDL stays low, and metabolic-syndrome risks pile on.
- Events rise: over years, odds of heart attack and stroke increase compared with people with healthier lipid patterns. (This is why guidelines focus on LDL/non-HDL reduction plus lifestyle, not just the HDL number.)
Quick FAQs
Does a high HDL cancel high LDL?
No. A high HDL doesn’t neutralize high LDL/non-HDL. You still need to lower the atherogenic particles that drive plaque.
How fast can HDL improve?
Triglycerides often respond in 2–4 weeks; LDL/non-HDL shift over 6–12 weeks of consistent habits. HDL tends to rise modestly and more slowly, while HDL function improves with the same habits. (Stay the course for months, not days.)
Should I start alcohol “for HDL”?
No. Even if alcohol nudges HDL up, it brings other risks. It isn’t a treatment for cholesterol. Stick to food, movement, and medically-guided therapy.
The takeaway
Low HDL is a red flag about the pattern, not just a number. Fix the pattern—move 150–300 min/week, lift twice weekly, swap to unsaturated fats, add soluble fiber and omega-3s, cut added sugars, stop smoking, and treat LDL/non-HDL to target. That’s how you lower real-world risk—and HDL usually follows.
Disclaimer
This article is for general education only and is not medical advice. Cholesterol targets, medications, and diet or exercise changes should be discussed with your doctor or a qualified dietitian, especially if you have heart disease, diabetes, kidney or liver conditions, or you are pregnant or breastfeeding.